Practical ways to develop leadership and management skills, experience and capabilities

On this page
Leadership development is highly personal and can be challenging. Trainers, supervisors and educators need to be able to support their trainees at each stage of development, including their readiness to learn from exposure to and engagement in different situations.
Trainees require support and encouragement from their trainers, supervisors and educators to navigate a range of leadership tasks and situations that aim to stretch and challenge them, coupled with meaningful, tailored feedback on their performance.
While those responsible for education, training and supervision may have gained leadership experience in different situations and contexts, if not in formal roles, they may have received little formal leadership development themselves. Therefore they may find it challenging to identify opportunities for leadership development and provide feedback to trainees. This guide aims to address this gap and provide ideas and examples for both trainers, supervisors, educators and trainees to engage routinely in leadership development in the workplace.
Workplace-based learning
Leadership opportunities and activities can be found everywhere in clinical and non-clinical situations for all healthcare professionals. Our survey of trainers and trainees found that the workplace is where doctors should primarily learn to develop their leadership capabilities in both clinical and non-clinical situations. This reflects the Center for Creative Leadership 70:20:10 model for learning and development:
- 70% of learning is gained from hands on experience in the workplace
- 20% from interaction with others (social learning)
- 10% from formal courses or training.
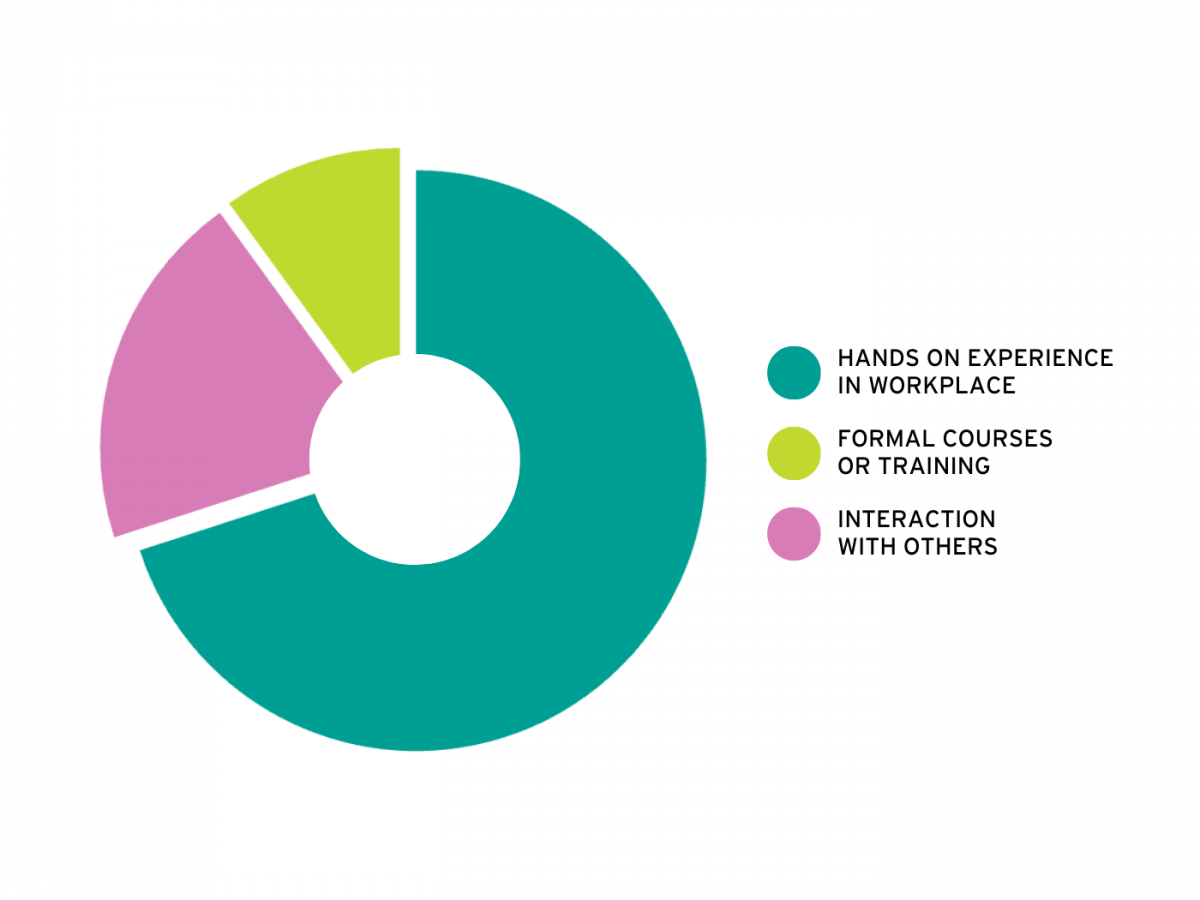
Recent thinking is more fluid and contextualised than a strict percentage, but ‘learning leadership’ involves a combination of on-the-job, social and formal learning. The task for trainers, educators, supervisors and trainees is to optimise learning and highlight connections through these three approaches.
In everyday practice, leadership involves a combination of what you do and how you do it.
In this section, **video examples** and case studies of useful developmental activities in which doctors in training have engaged and some ideas around how trainers and supervisors can hold meaningful professional conversations geared around leadership and management are presented.
Examples of workplace-based learning
Leadership activities can be fully integrated into everyday practice (such as leading a ward round, clinic, or team meeting) as well as being ‘over and above’ routine work (e.g. improvement projects or other leadership initiatives). The leadership activities in which doctors in training can (and should) engage will probably become increasingly complex and impactful as they progress through training. However, at any level, it is vital that doctors are exposed to activities which help develop:
- Understanding of how practices, departments, services, organisations, and systems work: structures, functions and cultures
- Awareness of how communications function and how decisions are made (formally and informally)
- Understanding of themselves, strengths, preferences and areas for development
- Skills in handling a range of clinical and managerial situations; being able to judge when to take leadership, when management is required, and when and how to follow
- Being able to work with people with different ideas, perspectives, and backgrounds to optimise engagement and inclusion and manage conflict appropriately.

How leadership and management skills are developed
Learning should be scaffolded according to stage of training and individual development, supported by relevant coaching and mentoring. Whilst leadership activities, learning and feedback should be embedded into all aspects of clinical work, it is often hard to understand how to use experiential learning in practice and when and how to engage in more formal learning opportunities. Petrie’s (2014, 2015) concepts of horizontal and vertical development provide a useful framework.
Horizontal development
Horizontal development (Petrie 2014, 2015) is all about adding new skills, capabilities and knowledge to a leader’s repertoire. It is an essential part of leadership development as it provides the underpinning concepts, models and tools. For example:
- if you are thinking about planning a change, knowing about some change models and being able to use management tools would be helpful
- if you are writing a reflection on an event or situation, a reflective model will help you to structure your thinking and writing
- if you are undertaking a quality improvement project, then learning about improvement methodologies will be essential.
Short courses or programmes (online or face to face) can be useful for providing an introduction to concepts and current thinking, knowledge transfer and for upskilling or learning about specific topics.
Longer programmes give more opportunities for networking and self and skill development and extended programmes help develop new mindsets, engage in in-depth discussions and deeper learning as well as recognise learning through a formal award.
Many programmes are blended or hybrid, with centralised e-learning to cover the theoretical basics and philosophy supplemented by local workshops. This approach can improve accessibility and enable more people to ‘learn leadership’.
Vertical development
Key to being and becoming an effective leader is the development of a mindset that is open to experiences, opportunities, ideas, perspectives, and growth. Such a mindset involves taking responsibility for one’s own learning, being curious and reflective about what is happening and why and being willing to identify and seek out opportunities for learning and personal growth.
Petrie (2014) suggests that vertical development for leadership requires exposure to ‘heat experiences’ (challenging or stimulating experiences), willingness to hear ‘colliding perspectives’ from colleagues from different professions, career stages and settings and supported, guided reflection to aid ‘sensemaking’.
Both the trainer and trainee need to work together to identify and seek out opportunities for development and to make time for reflection, feedback, and subsequent action.
The learning or developmental conversation is central to vertical leadership development because it involves helping the learner to process and make sense of their experiences and apply these insights to practice.
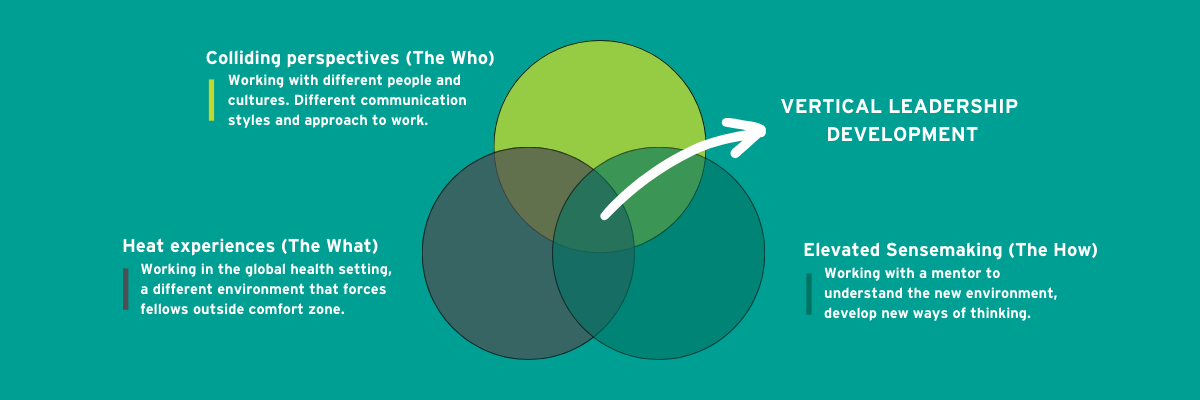
Heat experiences are situations where you might feel challenged, uncomfortable or uncertain. Doctors are trained to recognise and learn from clinical experiences throughout their training, learning from observation, reflection and conversation so that they are better equipped to manage an intense situation the next time. The same process can be applied to leadership development. Heat experiences (if used as part of a learning process) can provide you with an opportunity for the greatest growth.
Colliding perspectives involve actively and proactively exposing oneself to and interacting with people with different perspectives and ideas. It is the essence of inclusive leadership, where diversity of experiences and ideas are welcomed and nurtured. Role models and examples of good (and bad!) practice can come from many sources, in multi professional settings as well as outside the workplace. Supporting trainees to collaborate, work and learn together, for example through action learning sets or team projects can help provide extra support and feedback on leadership and management skills. Examples of learning approaches include shadowing junior/senior leaders; purposeful observation; small group discussions; case work/studies; mixing specialities, professions and occupations; embedding opportunities for reflective practice.
Sensemaking is the final part of vertical leadership development and is all about having conversations and reflecting about situations, how you operated, what impact you had on the situation, how other people might have felt or working out why they reacted or behaved in the way they did. As with other aspects of professional development, these reflections should lead you to a better understanding of the situations and help you decide to make changes in your behaviour or thinking and identify actions you can take, including horizontal development. Mentoring, coaching and action learning can all help support vertical development for leadership.
Horizontal and vertical leadership development work together and it will vary between individuals and their own experiences and needs. For example, you might go on a course and take learning from that to help you explore practical applications of the learning in the workplace. Alternatively, a heat experience might lead you to recognise that more knowledge or insight into what happened and how to manage it is required.
The associated resources provide different examples of how trainers and trainees have used this approach in practice to enhance their leadership development.
Section resources
Videos
Podcasts
Online talks
Brown, B. (2010) ‘The power of vulnerability’. Ted.com.
Edmonston, A. (2017). ‘How to turn a group of strangers into a team’. Ted.com.
Goleman, D. (2012) ‘Introduces Emotional Intelligence’. YouTube.
Reitz, M. (2017) ‘How your power silences truth’. YouTube.
Robertson, I. (2012) ‘Resilience: Factors that increase resilience’. YouTube.
Sinek, S. (2009). ‘How great leaders inspire action’. Ted.com.
Snowden, D. (2010) ‘The Cynefin Framework’. YouTube.
Websites
FMLM training and development hub
FMLM Leadership commitment for junior doctors
A doctor’s guide to everyday leadership
Networks
Record keeping
FMLM Leadership development passport
Annual review of competency progression (ARCP)
e-Learning
elearning for healthcare (2020) Management and Leadership Skills - elearning for healthcare.
Articles, books, reports
Aggarwal, R., and Swanwick, T. (2015). ‘Clinical leadership development in postgraduate medical education and training:Policy, strategy, and delivery in the UK national health service’, Journal of Healthcare Leadership, Vol. 7, pp. 109–12.
Allen, S. J. (2007). ‘Adult Learning Theory and Leadership Development’, Kravis Leadership Institute, Leadership Review(Vol. 7).
Baird, H., Malik, M., Patel, N., Yassaee, A. A., Tweedie, J., and Hynes, G. (2018). ‘Supporting junior doctors’ leadership:a trilogy of work’, BMJ Leader, 2(4), pp. 126–127.
Berghout, M. A., Fabbricotti, I. N., Buljac-Samardžić, M., and Hilders, C. G. J. M. (2017). ‘Medical leaders or masters?—A systematic review of medical leadership in hospital settings’, PLOS ONE, 12(9), pp. e0184522.
Beer M., Finnström, M., Schrader, D. (2016). ‘Why Leadership Training Fails—and What to Do About It’, Harvard Business Review, 94(10), pp. 50–57.
Beer, M., Finnstrom, M. and Schrader, D. (2016). ‘The Great Training Robbery: Working Paper’, Harvard Business School, pp. 16-121.
Blumenthal, D.M., Bernard, K., Bohnen, J. and Bohmer, R. (2012). ‘Addressing the leadership gap in medicine: residents' need for systematic leadership development training’, Academic Medicine, 87(4), pp. 513-522. DOI:10.1097/ACM.0b013e31824a0c47
Boak, G., Dickens, V., Newson, A., and Brown, L. (2007). ‘Distributed leadership, team working and service improvement in healthcare’, Leadership in Health Services, 28(4), pp. 332–344.
Bohmer, R. (2012). The instrumental value of medical leadership: Engaging doctors in improving services, The King’s Fund, London.
Burn, E., Waring, J. (2022). ‘The evaluation of health care leadership development programmes: a scoping review of reviews’, Leadership in Health Services, Ahead of print.
Caffarella, R. S., and Daffron, S. R. (2013). Planning programs for adult learners: A practical guide, John Wiley and Sons, Chichester.
Carroll, B., Nicholson, H. (2014). ‘Resistance and struggle in leadership development’, Human Relations, 67, pp. 1413-1436.
Center for Creative Leadership. (2022). ‘The 70-20-10 rule for leadership development’, Centre for creative leadership, Greensboro, NC.
Center for Creative Leadership. (2019). Benchmarking the state of leadership development: Today & tomorrow, Center for creative leadership, Greensboro, NC.
Center for Creative Leadership. (2021). ‘Leadership Development Research: What Works And What Doesn’t?’, Center for creative leadership, Greensboro, NC.
Cheng, E. W. L., and Hampson, I. (2008). ‘Transfer of training: A review and new insights’, International Journal ofManagement Reviews, 10, pp. 327–341.
Day, D. V. (2000). ‘Leadership development: A review in context’, The Leadership Quarterly, 11, pp. 581-613.
Day, D. V., Harrison, M. M., Halpin, S. M. (2009). An integrative approach to leader development: Connecting adult development, identity, and expertise, Psychology Press, New York
Day, D. V., Riggio, R. E., Tan, S. J., Conger, J. A. (2021). ‘Advancing the science of 21st- century leadership development: Theory, research, and practice’, The Leadership Quarterly, 32, pp.101557.
Day, D. V., Sin, H. P., Day, V. D., and Sin, H. P. (2011). ‘Longitudinal tests of an integrative model of leader development:Charting and understanding developmental trajectories’, Leadership Quarterly, 22(3), pp. 545–560.
DeRue, D. S., Wellman, N. (2009). ‘Developing leaders via experience: The role of developmental challenge, learning orientation, and feedback availability’, Journal of Applied Psychology, 94, pp. 859–875.
DeRue, D., Myers, C. G. (2014). Leadership Development: A review and agenda for future research. In D. V. Day (ed), The Oxford handbook of leadership and organisations, pp. 832-855, Oxford University Press, Oxford.
Fisher, E. S., Berwick, D. M., and Davis, K. (2009). ‘Achieving Health Care Reform — How Physicians Can Help’, New England Journal of Medicine, 360(24), pp. 2495–2497.
Fitzgerald, L., Ferlie, E., McGivern, G., and Buchanan, D. (2013). ‘Distributed leadership patterns and service improvement: Evidence and argument from English healthcare’, The Leadership Quarterly, 24(1), pp. 227–239.
Frich, J. C., Brewster, A. L., Cherlin, E. J., and Bradley, E. H. (2015). ‘Leadership Development Programs for Physicians: A Systematic Review’, Journal of General Internal Medicine, 30(5), pp. 656–674.
Ganz, M., Lee Cunningham, J., Ben Ezer, I., Segura, A. (2023). ‘Crafting public narrative to enable collective action: a pedagogy for leadership development’, Academy of Management Learning & Education, 22, pp. 169-190.
Geerts, J.M., Goodall, A.H. and Agius, S. (2020). ‘Evidence-based leadership development for physicians: a systematic literature review’, Social Science & Medicine, 246, pp.112709.
Goffee, R. and Jones, G. (2007). ‘Leading Clever People’, Harvard Business Review, 85(3), pp. 72-79.
Goodall, A. H., and Stoller, J. K. (2017). ‘The future of clinical leadership: evidence for physician leadership and the educational pathway for new leaders’, BMJ Leader, 1(2), pp. 8–11.
Hammond, M., Clapp-Smith, R., Palanski, M. (2017). ‘Beyond (Just) the workplace: A theory of leadership development across multiple domains’, Academy of Management Review, 42, pp. 481-498.
Hannum, K., Martineau, J., and Reinelt, C. (Eds.). (2007). The handbook of leadership development evaluation. Center for creative leadership, Greensboro, NC.
Haslam, S. A., Steffens, N. K., Peters, K., Boyce, R. A., Mallett, C. J., Fransen, K. (2017). ‘A social identity approach to leadership development’, Journal of Personnel Psychology, 16, pp. 113-124.
Ireri, S., Walshe, K., Benson, L., and Mwanthi, M. A. (2011). ‘A qualitative and quantitative study of medical leadership and management: experiences, competencies, and development needs of doctor managers in the United Kingdom’, Journal of Management and Marketing in Healthcare, 4(1), pp. 16–29.
Klimoski, R., Amos, B. (2012). Practicing evidence-based education in leader development, Academy of Management Learning & Education, 11, pp. 685-702.
Knowles, M. S., Holton, E. F., and Swanson, R. A. (2005). The adult learner: the definitive classic in adult education and human resource development (6th ed), Elsevier, London
Kumar, B., Swee, M. L., and Suneja, M. (2020). Leadership training programs in graduate medical education: A systematic review, BMC Medical Education, 20(1), 175.
Leslie, L. K., Miotto, M. B., Liu, G. C., Ziemnik, S., Cabrera, A. G., Calma, S., Huang, C., and Slaw, K. (2005). ‘Training young pediatricians as leaders for the 21st century’, Paediatrics, 115(3), pp. 765–773.
Lyons, O., George, R., Galante, J., Mafi, A., Fordwoh, T., Frich, J., and Geerts, J. (2020). ‘Evidence-based medical leadership development: a systematic review’, BMJ Leader, 5, pp. 206–213.
Maza, Y., Shechter, E., Pur Eizenberg, N., Segev, E. G., and Flugelman, M. Y. (2016). ‘Physician empowermentprogramme; a unique workshop for physician-managers of community clinics’, BMC Medical Education, 16(1), pp. 269.
Mezirow, J. (1978). ‘Perspective transformation’, Adult Education, 28(2), pp. 100–110.
Mianda, S., Voce, A. S. (2017). ‘Conceptualizations of clinical leadership: a review of the literature’, Journal of Healthcare Leadership, 9, pp. 79–87.
Mukhalalati, B. A., and Taylor, A. (2019). ‘Adult Learning Theories in Context: A Quick Guide for Healthcare ProfessionalEducators’, Journal of Medical Education and Curricular Development, 6, pp. 2382120519840332.
Narayandas, D., Moldoveanu, M. (2019). ‘The future of leadership development’, Harvard Business Review, 97, pp. 40–48.
Noordegraaf, M., E Schneider, M. M., J Van Rensen, E. L., and P E F Boselie, J. P. (2015). Cultural Complementarity:Reshaping professional and organizational logics in developing frontline medical leadership, Public ManagementReview, 18(8), pp. 1111-1137.
Pearce, C. L., Manz, C. C., and Sims, H. P. (2009). Where Do We Go From Here?. Is Shared Leadership the Key to Team Success?, Organizational Dynamics, 38(3), pp. 234–238.
Perry. J., Mobley, F., Brubaker, M. (2017). ‘Most doctors have little or no management training and that’s a problem’, Harvard Business Review, 15 December.
Petrie, N. (2014). ‘Future trends in leadership development [White Paper]’, Center for creative Leadership, Greensboro, NC.
Petrie, N. (2015). ‘The How-To of Vertical Leadership Development – 30 Experts, 3 Conditions, and 15 Approaches’, Center for creative Leadership, Greensboro, NC.
Petrie, N. (2014). ‘Vertical Leadership Development–Part 1 Developing Leaders for a Complex World’, Center for creative Leadership, Greensboro, NC.
Petriglieri, G., Wood, J. D., Petriglieri, J. L. (2011). ‘Up Close and Personal: Building Foundations for Leaders' Development Through the Personalization of Management Learning’, Academy of Management Learning & Education,10, pp. 430–450.
Podolny, J. M. (2011). ‘A conversation with James G. March on learning about leadership’, Academy of Management Learning & Education, 10, pp. 502-506.
Rabin, R. (2014). ‘Blended Learning for Leadership: The Centre for Creative Leadership Approach’, Center for creative Leadership, Greensboro, NC.
Reeve, J., and Jang, H. (2006). ‘What teachers say and do to support students’ autonomy during a learning activity’,Journal of Educational Psychology, 98(1), pp. 209–218.
Rooke, D. (2018). ‘Transformational leadership capabilities for medical leaders’, BMJ Leader, 2, pp. 3-6.
Rooke, D. and Torbert, W. (2005). ‘Seven transformations of leadership’, Harvard Business Review, 83(4), pp. 66-76.
Sadowski, B., Cantrell, S., Barelski, A., O’Malley, P. G., and Hartzell, J. D. (2018). ‘Leadership Training in GraduateMedical Education: A Systematic Review’, Journal of Graduate Medical Education, 10(2), pp. 134–148.
Sarto, F. and Veronesi, G. (2016). ‘Clinical leadership and hospital performance: assessing the evidence base’, BMC health services research, 16, pp. 85-97
Savage, M., Savage, C., Brommels, M., and Mazzocato, P. (2020). ‘Medical leadership: boon or barrier to organisational performance? A thematic synthesis of the literature’, BMJ Open, 10(7), pp. e035542.
Schön, D. A. (1987). Educating the reflective practitioner, Jossey-Bass, New Jersey
Snowden, D.J. and Boone, M.E. (2007). ‘A Leader's Framework for Decision Making’, Harvard Business Review, 85(11), pp. 68-76, 149.
Straus, S. E., Soobiah, C., and Levinson, W. (2013). ‘The impact of leadership training programs on physicians inacademic medical centers: A systematic review’, Academic Medicine, 88(5), pp. 710–723.
Sultan, N., Torti, J., Haddara, W., Inayat, A., Inayat, H., and Lingard, L. (2019). ‘Leadership Development in PostgraduateMedical Education: A Systematic Review of the Literature’, Academic Medicine, 94(3), pp. 440–449.
Swanwick T, and McKimm J. (2012). ‘Clinical leadership development: requires system-wide interventions, not just courses’, The Clinical Teacher, 9(2), pp. 89-93.
Swanwick, T. and McKimm, J. (2017) ABC of Clinical Leadership, Wiley-Blackwell, New Jersey
Tasi, M., Keswani, A., and Bozic, K. (2019). Does physician leadership affect hospital quality, operational efficiency, and financial performance?, Health Care Management Review, 44(3), pp. 256-262.
Taylor, D. C. M., and Hamdy, H. (2013). ‘Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83’, Medical Teacher, 35(11), pp. e1561-e1572.
Vogel, B., Reichard, R. J., Batistič, S., Černe, M. (2021). ‘A bibliometric review of the leadership development field: How we got here, where we are, and where we are headed’, The Leadership Quarterly, 32, pp. 101381.
Vongswasdi, P., Leroy, H., Anisman-Razin, M., Claeys, J., Van Dierendonck, D. (2023). ‘Beyond Developing Leaders: Toward a Multi-Narrative Understanding of the Value of Leadership Development Programs’, Academy of Management Learning & Education.
Wallace, D. M., Torres, E. M., Zaccaro, S. J. (2021). ‘Just what do we think we are doing? Learning outcomes of leader and leadership development’, The Leadership Quarterly, 32, pp. 101494.
West, M., Armit, K., Loewenthal, L., Eckert, R., West, T., and Lee, A. (2015) ‘Leadership and Leadership Development in Health Care: The Evidence Base’, The Kings Fund, pp. 1–36.
