Better decision-making for aspiring medical leaders
As a Cardiology trainee, I sat my specialty certificate exam, the European Examination in Core Cardiology (EECC)[1], last year. I followed my usual study technique, memorising facts, guidelines and examples of mock questions and answers. Having gone through similar assessments for over a decade now, I have had some time to pause and reflect on the differences in decision-making between choosing ‘A’ or ‘B’ in a multiple choice format, and the actual decision-making that I practice whilst working in clinic, on-call or in a leadership setting.
A central thought I had was that the summative assessments clinicians face often frame complex problems with the certainty of ‘a single best answer’ that does not exist in the real world, even when following guidelines of best practice.[2] The National Institute for Health and Care Excellence (NICE) captures this with “guidance does not override the individual responsibility of health professionals to make appropriate decisions according to the circumstances of the individual patient in consultation with the patient”. [3]
Nevertheless, clinical guidelines frequently do offer granular detail of ‘what to do in typical scenarios’, eg measure levels of NT-proBNP in patients with suspected acute heart failure [NICE CG187]. And this ‘how to’ guide taps deep into the psyche of what clinicians seek whenever confronted with uncertainty and risk – reassurance that what we do is ‘within recommended practice’. Yet for non-clinical decisions required of medical leaders, the granular detail of ‘what to do’ is simply not available and instead only general recommendations and standards exist [4].
Decision-making ambiguity is therefore almost always amplified in leadership roles and can be particularly tough for junior doctors to navigate, given their lack of formal training or experience in dedicated leadership positions. Step-by-step guidance is lacking, and even if they were produced, aspiring medical leaders must be mindful of avoiding blind adherence to such guidance which cannot be prescriptive to each unique situation.
Thinking about leadership and decision-making
I wish to challenge readers to think more deeply about the topic of decision-making as applied to medical leadership. I have zoomed-in on two aspects of this vast landscape, offering a brief discussion of:
- How and why decisions made by medical leaders may differ from decisions made in a clinical context, and
- How to ‘train’ to become a leader who takes better decisions, noting that the path is not linear and that tools such as perspective taking and mentorship [5] are vital in exploiting lived experience and lessons learnt from wider reading, leadership courses or feedback received.
1. Making decisions as a clinician versus making decisions as a leader
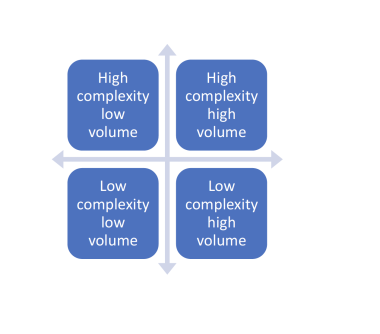
Decision-making in medicine encompasses a wide range of calls to make, regardless of specialty or setting. Figure 1 categorises decision-making across a spectrum of volume and complexity.
I would contend that although clinicians may vary considerably in assessing how their own decisions may fall into the above framework, the variation among medical leaders is likely to be greater. In addition, instead of answering simple AB questions, such as whether to prescribe a balanced crystalloid solution, or normal saline, the scope of questions and choice of answers for most medical leaders is also far greater. As a top line example, setting a new or refreshed vision for a team, department or organisation cannot be reduced to a simple A versus B choice.
The lack of a traditional evidence base (eg RCT level data) to inform leaders of what to do comes with this territory, although it is balanced with (usually) more time to evaluate choices and to assemble a diverse team to pool expertise and harness the wisdom of a collective before deciding on a course of action.
Although the routine work of clinicians, such as running a ward round or medical clearly involves both medical and leadership decisions, the purpose in drawing a distinction between the two is to consider what cognitive biases or traps in thinking may particularly affect decision makers in each role. To take just two examples, decision fatigue (more likely when the volume of decisions increase) and blind-spot bias (more likely in complex decision spaces) may have vastly different likelihoods and impact, depending on the context. This simple act of thinking about how decisions can be distorted represents an important step on the journey to becoming a more effective decision-maker in any context. For interested readers, a good primer on common cognitive biases can be found here - https://qualitysafety.bmj.com/content/22/Suppl_2/ii58
The role of a medical leader also involves handling a different type of risk compared to that encountered in a clinical role – not the immediate ‘make a correct diagnosis or ‘lead the resuscitation team’ but a broader level of accountability for delivery of, for example, a project, a course, a standard or even the performance of a department or a hospital. For aspiring medical leaders, this is not something that is ‘assessable’ in an exam, nor explicitly trainable as part of a curriculum. Perhaps here the value of reflexivity, mentorship and seeking advice are simple yet effective ways of beginning to learn the ropes of risk handling in a leadership context.
2. Perspective taking and leadership training
In my early career, I was lucky enough to be in the right place at the right time to have taken on a formal leadership role. As the RCP Chief Registrar at St Bartholomew’s hospital, I juggled clinical commitments with days working on distinct projects relevant to the hospital, or engaging in meetings with various managers and clinical leaders. The experience gave me plenty to think about in terms of how different elements of the healthcare system require individuals to execute radically different types of decisions. As someone with a medical background, I appreciated how certain traits were echoed by decision-makers I met, regardless of their professional background, such as the art of problem solving through pattern recognition, as well as the importance of effective and timely communication. The unique opportunity to see things from a different perspective was invaluable and I would recommend to any interested reader to seek out opportunities whenever you have the headspace to do so, or to explore your curiosity at work with simple habits such as engaging with your non-medical colleagues – these subtle shifts in your behaviour may lead to bigger effects later in your career!
What I remember most vividly during my time is the manner in which effective leaders took important decisions. The adage ‘people remember how they were made to feel rather than what was said’ fits with my own view that a collaborative approach which may not be spot-on is often better than an aggressive approach, especially as decisions are not usually taken in isolation and most circumstances change, often requiring iteration of original actions.
One other key trait of effective leaders I saw was explicitly double-checking for the Dunning-Kruger effect. [6] In other words, ensuring that the confidence with which you hold your view is well-calibrated to the accuracy of that view, and avoiding being ‘wrong and strong’. I find this quite difficult to do consistently, and to some extent we’re always going to be under or over-confident. Nicole Treadway wrote a salient piece on confidence and was interviewed about it here- https://www.medscape.com/viewarticle/906878. I have found there are many popular science books available to begin thinking about your own calibration, though Julia Galef’s Scout Mindset is perhaps the best place to start. [7]
Returning to assessments and training, I wish to close with the argument that the essential traits and training required of a leader or aspiring leader is focused too much on the individual. The idea of seeking a second, third or group opinion is familiar to all clinicians when considering complex decisions presented in a multidisciplinary team (MDT) meeting, yet apart from this outlier, the idea of group performance and seeking peer review of our own decisions is pretty alien to our existing training and assessment paradigms, particularly in clinical contexts.
While effective leaders and clinicians both require a willingness to take on board views from others, the skill of being 'confidently unconfident’ and displaying a willingness to seek feedback and alternative views is underused in many settings I’ve worked in. Perhaps that is because there aren’t enough of us around, but I think there is another reason too – we are so used to either following guidelines of best practice or ‘differentiating that option B is better than A’ in a solo exam, that we don’t wish to admit that the real world is not as certain as what we read in text or in what we need to portray in order to live up to our image as ‘expert professionals' who can single-handedly solve the problem.
Perhaps far more than we realise or know, there is no single best answer for the decision, just a course of action that once taken, requires reflection, analysis and openness to timely course correction if better options emerge. Hopefully some interesting food for thought for any aspiring medical leader, and a nice break from preparing for the next single best answer examination.
Dr Yang Chen BMBCh MA MRCP MSc, Cardiology Registrar and FMLM Founding Associate Fellow
@DrYangChen
References
- European Society of Cardiology. European Exam in Core Cardiology (Online). Available at: https://www.escardio.org/Education/Career-Development/European-Exam-in-Core-Cardiology-(EECC) Accessed on: 12 March 2022.
- Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M et al. ESC Scientific Document Group. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021 Sep 7;42(34):3227-3337.
- The guidelines manual. National Institute for Health and Care Excellence. 2012. Available at: https://www.nice.org.uk/process/pmg6/chapter/introductionAccessed on 20 February 2022.
4. Faculty of Medical Leadership and Management. Leadership and Management Standards for Medical Professionals. (Online). Available at: https://www.fmlm.ac.uk/standards Accessed on 11 March 2022.
5. Mohammed R. Faculty of Medical Leadership and Management Blog (Online).Available at: https://www.fmlm.ac.uk/news-opinion/blog/mentoring-the-key-to-growth-and-development Accessed on 9 March 2022.
6. Mazor, M., Fleming, S.M. The Dunning-Kruger effect revisited. Nat Hum Behav 5, 677–678 (2021)
7. Galef J. The Scout Mindset: Why Some People See Things Clearly and Others Don't. Penguin; 2021 Apr 13